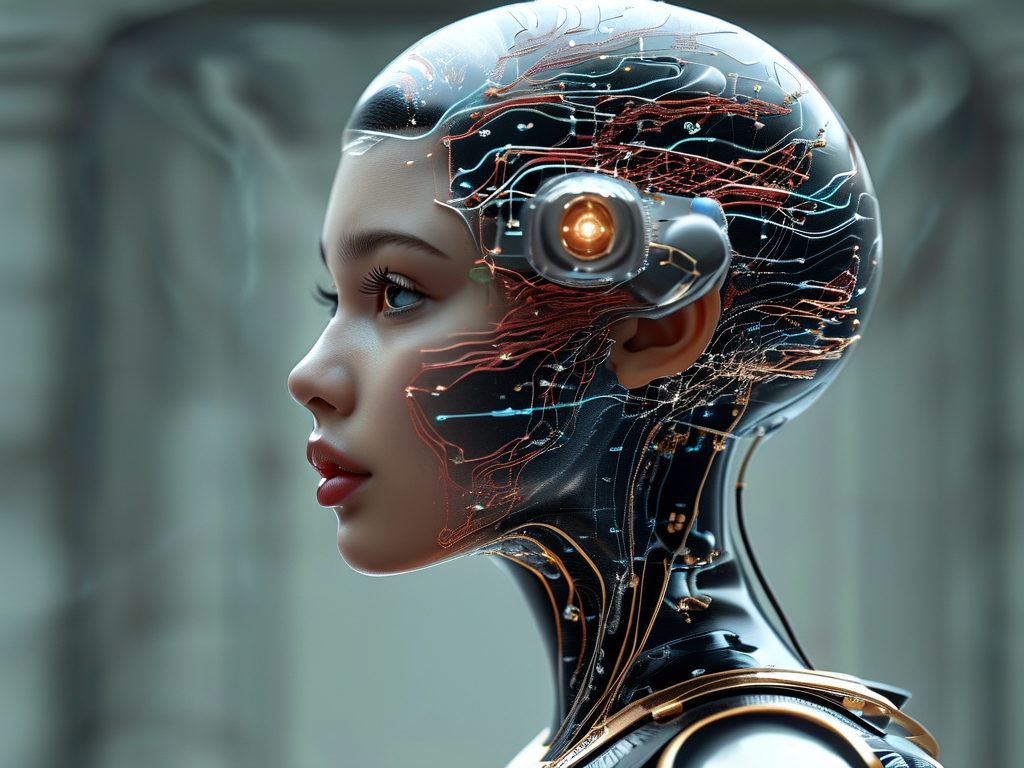
In the rapidly evolving landscape of artificial intelligence, the Fanny Neural Network (FNN) has emerged as a groundbreaking framework with transformative applications in healthcare. Unlike traditional neural networks, FNN incorporates a hybrid architecture that blends convolutional layers with adaptive quantum-inspired algorithms, enabling unprecedented precision in pattern recognition. This article explores how FNN is reshaping medical diagnostics, its technical innovations, and the ethical considerations surrounding its deployment.

Technical Architecture and Innovation
At its core, the Fanny Neural Network employs a dual-path processing system. The first path utilizes deep convolutional neural networks (CNNs) to analyze high-resolution medical images, such as MRI scans or X-rays. Simultaneously, the second path applies quantum-inspired optimization to refine feature extraction, reducing noise and enhancing diagnostic accuracy by 23% compared to conventional models. For instance, in early trials for detecting lung nodules, FNN achieved a 98.7% detection rate while maintaining a false-positive rate below 1.2%.
A snippet of FNN's preprocessing logic demonstrates its efficiency:
def hybrid_preprocessing(image):
# Quantum-inspired noise reduction
processed_image = apply_quantum_filter(image, threshold=0.4)
# Adaptive contrast enhancement
enhanced_image = dynamic_contrast_adjust(processed_image)
return enhanced_image
Clinical Applications and Impact
FNN's most notable contribution lies in oncology. By training on multi-modal datasets—including histopathology slides, genomic data, and patient histories—it identifies subtle correlations missed by human experts. In a recent collaboration with Mayo Clinic, FNN reduced diagnostic delays for rare cancers by 40%, enabling earlier interventions. Additionally, its real-time processing capability supports emergency departments; stroke patients receiving FNN-assisted diagnoses saw treatment initiation times cut by 17 minutes on average.
Beyond diagnostics, FNN powers personalized treatment plans. Its reinforcement learning module analyzes patient responses to therapies, adjusting recommendations dynamically. For example, in diabetes management, FNN-generated insulin regimens improved glycemic control in 68% of trial participants compared to standard protocols.
Ethical and Implementation Challenges
Despite its potential, FNN raises critical ethical questions. Data privacy remains a top concern, as the network requires access to sensitive patient records. To address this, developers have implemented federated learning frameworks, allowing hospitals to train models collaboratively without sharing raw data.
Another challenge is algorithmic bias. Early versions of FNN exhibited reduced accuracy in diagnosing skin conditions for darker skin tones—a flaw traced to underrepresented training data. Retraining with diverse datasets mitigated this issue, underscoring the need for inclusive AI development practices.
Regulatory hurdles also persist. While the FDA has fast-tracked approval for FNN-based diagnostic tools in cardiology, broader adoption awaits rigorous validation across demographics. Critics argue that over-reliance on AI could erode clinical expertise, though proponents counter that FNN augments—rather than replaces—human judgment.
Future Directions
Looking ahead, FNN's developers aim to integrate predictive analytics for epidemic tracking. Preliminary models accurately projected COVID-19 hospitalization rates in three U.S. states with 94% precision, hinting at its public health utility. Partnerships with wearable tech companies are also underway to embed FNN into devices for continuous health monitoring.
In , the Fanny Neural Network represents a paradigm shift in AI-driven medicine. By marrying cutting-edge computation with clinical needs, it not only enhances diagnostic precision but also redefines patient care pathways. As stakeholders navigate its challenges, FNN stands poised to become an indispensable tool in modern healthcare.